Anesthetics are among the most commonly administered drugs in health care, as thousands of people are put under every day during painful procedures and surgery. What many people don’t realize is that anesthesia can have neurotoxic effects on the brain and contribute to environmental damage.
A team of Â鶹´«Ă˝ researchers and engineers are working to make anesthesia safer and cleaner. With help from the Rowe School of Business and the Brain Repair Centre, the team is hoping to introduce new anesthesia technology to the commercial market.
“What is the most pressing problem in health care?” asks Dr. Michael Schmidt. To him, the answer lies in an aging population, which is most susceptible to the often-deleterious effects of anesthesia.
Dr. Schmidt is an anesthesiologist at Capital Health, a professor at Â鶹´«Ă˝ Medical School, and a researcher who emigrated from Germany to Canada to continue to develop a safer system for anesthesia. “The motto for my research was, and is, to make anesthesia safer,” he says.
A safer, cheaper, greener solution
Current methods of general anesthesia require carbon dioxide (CO2) scrubbing, where the chemical used interacts with the anesthesia drugs to produce neurotoxic factors. These, along with the impact of the surgery itself, can result in postoperative cognitive decline. This phenomenon leaves patients with impaired cognitive function for weeks or months after surgery — and, in persistent cases, increases the risk of death.
Dr. Schmidt’s research is focused on reducing and eliminating this effect, which is especially important for an aging population, as those over 65 years are most susceptible to long-term cognitive problems after anesthesia and surgery.
Dr. Schmidt has teamed up with Florentin Wilfart, a biomedical engineering PhD student, to develop a commercially viable device that offers neuroprotection alongside anesthesia delivery. Wilfart and Dr. Schmidt have developed a device set to replace current CO2 scrubbing devices as it removes CO2 without producing neurotoxic compounds. This means the anesthetic drug can be delivered with less continual dilution and renewal, substantially reducing the amount of drug required. Not only does this save the health-care system money, it saves the environment from greenhouse gases 3,000 times more harmful than CO2.
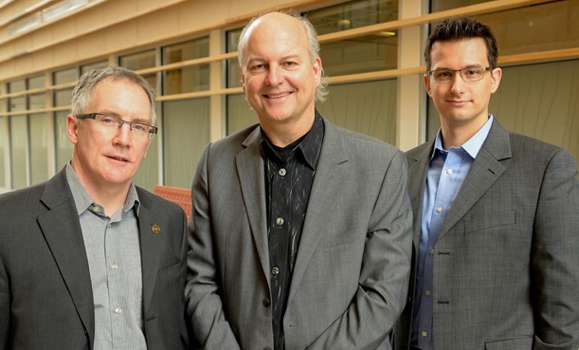
After only a couple years of development, Dr. Schmidt and Wilfart contacted David Roach, an assistant professor at Â鶹´«Ă˝â€™s Rowe School of Business. The trio went on to launch DMF Medical Inc., a startup company that has attracted funding for the testing and commercialization of their device. The team hopes to begin clinical trials of the new CO2-scrubbing device on humans later this year. The new technology could be implemented in operating rooms around the world as early as 2015.Â
New avenues to neuroprotection
This March, Dr. Schmidt received a knowledge translation grant from the Brain Repair Centre (BRC) to pursue another potential line of neuroprotective products based on his longstanding interest in the use of noble gases in anesthesia.
The Brain Repair Centre established its knowledge translation grants in 2013 to “provide an opportunity for scientists to take their innovations and push them forward in a way that will attract businesses and private funding,” explains Dr. Victor Rafuse, director of the Brain Repair Centre.
According to Dr. Schmidt, “The Brain Repair Centre knowledge translation grant will enable us to gather preliminary data on using noble gases as neuroprotectants, and go the next step and protect the intellectual property.”
Dr. Schmidt began his work on noble gases back in Germany, by looking at xenon. “Xenon appears as an almost ideal anesthetic,” he explains. “It can be used in surgery with almost no side effects, and you can use it on people who have a weak heart. It’s also a neuroprotectant; it can help protect the brain and the spinal cord during anesthesia.”
Unfortunately, xenon is rarely used, due to its prohibitive cost and the special technology needed for administration of the gas. Dr. Schmidt began looking at other noble gases, with neuroprotective properties similar to xenon, but far less costly to obtain.
Dr. Schmidt believes that adding noble gases to the mix during anesthesia may be an efficient way to protect the nervous system of patients under general anesthesia. “The Brain Repair Centre grant will help us explore the feasibility and cost-effectiveness of using noble gases in this way.”

