John Frampton arrived in the lab a few years ago to clean up after a failed experiment he’d carried out the day before. The biomedical engineer had been attempting to isolate a rare type of cell, but the technique he used in the experiment backfired and instead of separating from one another as he’d hoped, the different cells all gathered in the middle of his test tube.
Feeling frustrated by the previous day’s setback, Dr. Frampton was in the process of disposing of the materials he had left in an incubator overnight when he noticed something unexpected.
“When I dumped out the tubes, the cells had formed a little tissue at the interface,” remembers Dr. Frampton, who was a post-doctoral researcher at the University of Michigan at the time.
At some point between when Dr. Frampton left the lab and when he returned the following day, the microscopic cells had assembled together into a small piece of tissue without any manipulation at all. Dr. Frampton’s team was one of the first to show this kind of “self-assembly” could happen simply by letting cells float around in liquid polymer solutions, a technique that mimics the three-dimensional environment of an organ rather than the two-dimensional surface of a petri dish.
Recognizing opportunities
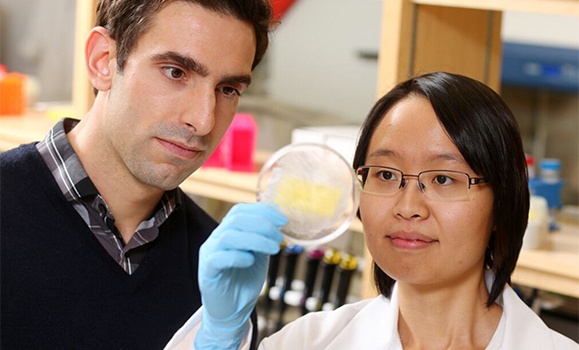
Since his accidental discovery, Dr. Frampton has figured out a way to speed up the process of creating the tissues in as little as two hours and is now collaborating with a colleague in the biomedical engineering department at Dal — which he joined as an assistant professor in 2014 — on a way to use the material in an application for helping to treat burns and other skin wounds. In Dr. Frampton’s case, failure gave way to opportunity.
“That can be how a lot of things come about. The key is to find the right people who can recognize those opportunities,” says the 31-year-old professor, who was awarded a tier-two, five-year Canada Research Chair grant worth $500,000 earlier this year for his work on tissue engineering and replacement.
Along with the Canada Research Chair funding, Dr. Frampton received a Canada Foundation for Innovation grant this year that he has used to outfit his lab in the Tupper Medical Building with special microscopes and other tools not available elsewhere at Dal. NSRIT provided matching funds in the amount of $124,849, and the total project amount was $327,770.
In addition to coming up with better ways to create lab-grown microscale tissues in three-dimensions, Dr. Frampton’s research group at Dal looks at a whole range of other issues, including what factors influence the ability of those lab-grown materials to successfully connect with the body after they are implanted.
Dr. Frampton’s research team takes an integrated approach to science and is made up of both graduate and undergraduate students from a host of different backgrounds, including neuroscience, engineering, immunology and even computer science. That multidisciplinary mix brings in the kind of new perspectives needed in biomedical engineering, which is all about applying engineering principles to medical problems.
Undergrads volunteer in the lab on a more casual basis, working on projects linked to the materials side of the research. Dr. Frampton says the hope is that they enjoy working in the lab that they decided to stick around and do a master’s with him.
A team approach
That’s what happened with Kristin Ko, a Dal neuroscience grad who worked in Dr. Frampton’s lab part-time last year before deciding to dive into a masters with him this year.
Ko first met Dr. Frampton, who also started out in neuroscience, last summer when he moved into the lab across the hall from the one where she did her honours thesis. She was taking a year off to explore her grad school options and passed him her resume one day in the hall.
“It was pretty interesting to find someone else who transitioned from neuroscience to biomedical engineering,” says Ko, who is using three-dimensional cell cultures to help shine a light on neurodegenerative disorders such as Parkinson’s Disease.
She cites Dr. Frampton’s “expertise in the field” and his ability to ask the right questions for helping her turn a really obscure idea into a manageable masters thesis project, which in turn helped her secure full funding for her first year of study and partial for her second year.
Making progress
While the hope is that Dr. Frampton and researchers like Ko can create technologies that make it into clinics, the professor admits the process can be painstaking and doesn’t always yield results right away.
“My hope is that if they don’t make it to clinic as a product then they may at least inspire a line of research that could lead to a product eventually or help some other product out there to provide better treatment,” says Dr. Frampton.
That kind of incremental progress could discourage some, but Dr. Frampton knows from first-hand experience just how important those smaller achievements can be in his field. He worked with two grad students during his post-doc at the University of Michigan to create a now-patented technology that helps confine antibodies in polymer systems, a technique he plans to use as one of the tools for analysis in his lab here at Dal. The grad students went on to form a start-up to sell the technology, which could eventually make its way into labs around the world.
“My hope is that as we develop a lot of these new things in the lab, we’ll start to think about ways we can commercialize,” says Dr. Frampton. “Maybe we’re not always developing new transplant material, but we’re developing something else that can fit into the drug discovery pipeline or somewhere else.